Abstract and Introduction
Introduction
In 2018, a total of 9,029 new tuberculosis (TB) cases were reported in the United States, representing a 0.7% decrease from 2017.* The U.S. TB incidence in 2018 (2.8 per 100,000 persons) represented a 1.3% decrease from 2017; the rate among non–U.S.-born persons was >14 times that in U.S.-born persons. This report summarizes provisional TB surveillance data reported to CDC's National Tuberculosis Surveillance System (NTSS) through 2018. Although the total number of cases and incidence are the lowest ever reported in the United States, a recent model predicted that the U.S. TB elimination goal (annual incidence of <1 case per 1 million persons) will not be attained in the 21st century without greatly increased investment in detection and treatment of latent TB infection (LTBI).[1] Programs to identify, test, and treat populations at high risk for TB remain important to eliminating TB in the United States.
Health departments in the 50 states and District of Columbia (DC) electronically report provisional case data that meet the national TB surveillance case definition to CDC.† Data reported include demographic information (e.g., birth date, sex, self-reported race/ethnicity, and country of birth), clinical information (e.g., reason for TB evaluation, anatomic site of disease, test results, and therapy administered), and information on TB risk factors (e.g., human immunodeficiency virus [HIV] infection status, history of homelessness, and residence in a congregate setting). According to U.S. Census Bureau definitions, a "U.S.-born" person is classified as one born in the United States or a U.S. territory or born abroad to a U.S. citizen parent. Race/ethnicity data are collected and reported using federal classification standards; Hispanics/Latinos can be of any race, and all other reported race categories are non-Hispanic/Latino. CDC derived the denominators used to calculate national and state TB incidence from July 2018 U.S. Census Bureau population estimates[2] and the denominators used to calculate TB incidence by national origin and race/ethnicity from July 2018 Current Population Survey data.[3] The number of reported TB cases and TB incidence (cases per 100,000 persons) for 2017 and 2018, as well as the percent changes from 2017 to 2018, were calculated for the 50 states and DC and for each U.S. Census Bureau division. The numbers of TB cases and TB incidence per 100,000 persons were calculated by national origin and race/ethnicity for 2015–2018.
TB incidence declined 1.3% from 2017 to 2018 and an average of 1.6% per year during the last 4 years (2014–2018), a slower pace of decline than the 4.7% annual decline during 2010–2014.§ State-specific TB incidence for 2018 ranged from 0.2 per 100,000 in Wyoming to 8.5 in Alaska, with a median rate of 1.9 (Table 1). Ten states (Alaska, California, Florida, Hawaii, Maryland, Massachusetts, Minnesota, New Jersey, New York, and Texas) and DC reported TB incidence above the national rate. As has been the case for over 2 decades, four states (California, Florida, New York, and Texas) accounted for approximately half of the reported cases of TB in the United States.
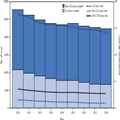
Among the 9,029 TB cases reported in the United States in 2018, approximately two thirds (6,276 [69.5%]) occurred in non–U.S.-born persons, whereas 2,662 (29.5%) occurred in U.S.-born persons; 91 (1.0%) cases occurred in persons for whom no national origin was documented (Table 2). This distribution is similar to that in 2017, when 6,392 (70.3%) cases occurred in non–U.S.-born persons, 2,693 (29.6%) occurred in U.S.-born persons, and 9 (0.1%) occurred in persons for whom no national origin was documented. TB incidence among non–U.S.-born persons (14.2 cases per 100,000) decreased by 3.8% from 2017 to 2018, and the incidence among U.S.-born persons (1.0 cases per 100,000) decreased by 1.8% (Figure).¶
Figure.
Number of tuberculosis (TB) cases and TB incidence, by national origin*,† — United States, 2010–2018
*Number of cases among non–U.S.-born and U.S.-born persons and associated incidence exclude cases with unknown country of origin. Incidence for all U.S. TB cases includes cases with unknown country of origin.
†Incidence for non–U.S.-born and U.S.-born persons calculated using population estimates from Current Population Survey. Incidence for all persons with TB diagnosed in the United States calculated using population estimates from U.S. Census Bureau.
Among non–U.S.-born persons with TB, incidence in 2018 was highest among Asians, followed by Native Hawaiians/Pacific Islanders, non-Hispanic blacks (blacks), Hispanics, and American Indian/Alaska Natives, and was lowest among non-Hispanic whites (whites) (Table 2). Among TB cases in non–U.S.-born persons, incidence decreased from 2017 to 2018 among Asians, blacks, and whites, but increased in Hispanics. The top five countries of birth of non–U.S.-born persons with TB were Mexico (1,195 cases; 19.0% of all non–U.S.-born cases), Philippines (781; 12.4%), India (616; 9.8%), Vietnam (503; 8.0%), and China (374; 6.0%). Among TB cases in non–U.S.-born persons, 2,905 (46.3%) were diagnosed ≥10 years after the patient first arrived in the United States.
The highest TB incidence for U.S.-born persons occurred among Native Hawaiians/Pacific Islanders, followed by American Indians/Alaska Natives, blacks, Asians, and Hispanics, and was lowest in whites (Table 2). Among U.S.-born persons, TB incidence decreased from 2017 to 2018 among blacks, but remained stable among Asians, Hispanics, and whites.
During 2018, 4.1% of TB cases were reported among persons who experienced homelessness within the year preceding diagnosis, 3.3% among residents of a correctional facility at the time of diagnosis, and 1.6% among residents of a long-term care facility at the time of diagnosis.** Among cases diagnosed in persons who experienced homelessness and among residents of long-term care facilities, 60.8% and 56.8%, respectively, were in persons who were U.S.-born, whereas among residents of a correctional facility, only 33.6% were U.S.-born. HIV status was known for 85.3% of TB cases reported in 2018. Overall, 5.3% of TB patients with known HIV status were coinfected with HIV, including 8.6% among persons aged 25–44 years.
Initial drug-susceptibility testing for at least isoniazid and rifampin was performed for 73.5% of all TB cases (and 93.8% of culture-confirmed cases) in 2017, the most recent year for which complete data are available.†† Among the 6,684 TB cases reported in 2017 with available drug-susceptibility testing results, 128 (1.9%) were multidrug-resistant TB.§§ Of these multidrug-resistant TB cases, 110 (85.9%) were in non–U.S.-born persons; 26 (20.3%) multidrug-resistant TB patients reported a previous episode of TB. Three cases of extensively drug-resistant TB¶¶ were reported, all of which occurred in non–U.S.-born persons.
Morbidity and Mortality Weekly Report. 2019;68(11):257-262. © 2019 Centers for Disease Control and Prevention (CDC)