While cases of syphilis in Europe were first recorded over 500 years ago, no vaccine candidates have ever advanced to human clinical trials. A new international, multi-university center led by the University of Connecticut School of Medicine and the Connecticut Children’s Medical Center aims to change that.
The University of Connecticut will receive up to $11 million over five years from the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH) to develop a vaccine for this centuries-old disease.
Syphilis poses serious health consequences internationally and in the United States. The World Health Organization (WHO) estimates that 10.7 million people between the ages of 15 and 49 had syphilis in 2012, and about 5.6 million people contract it every year.
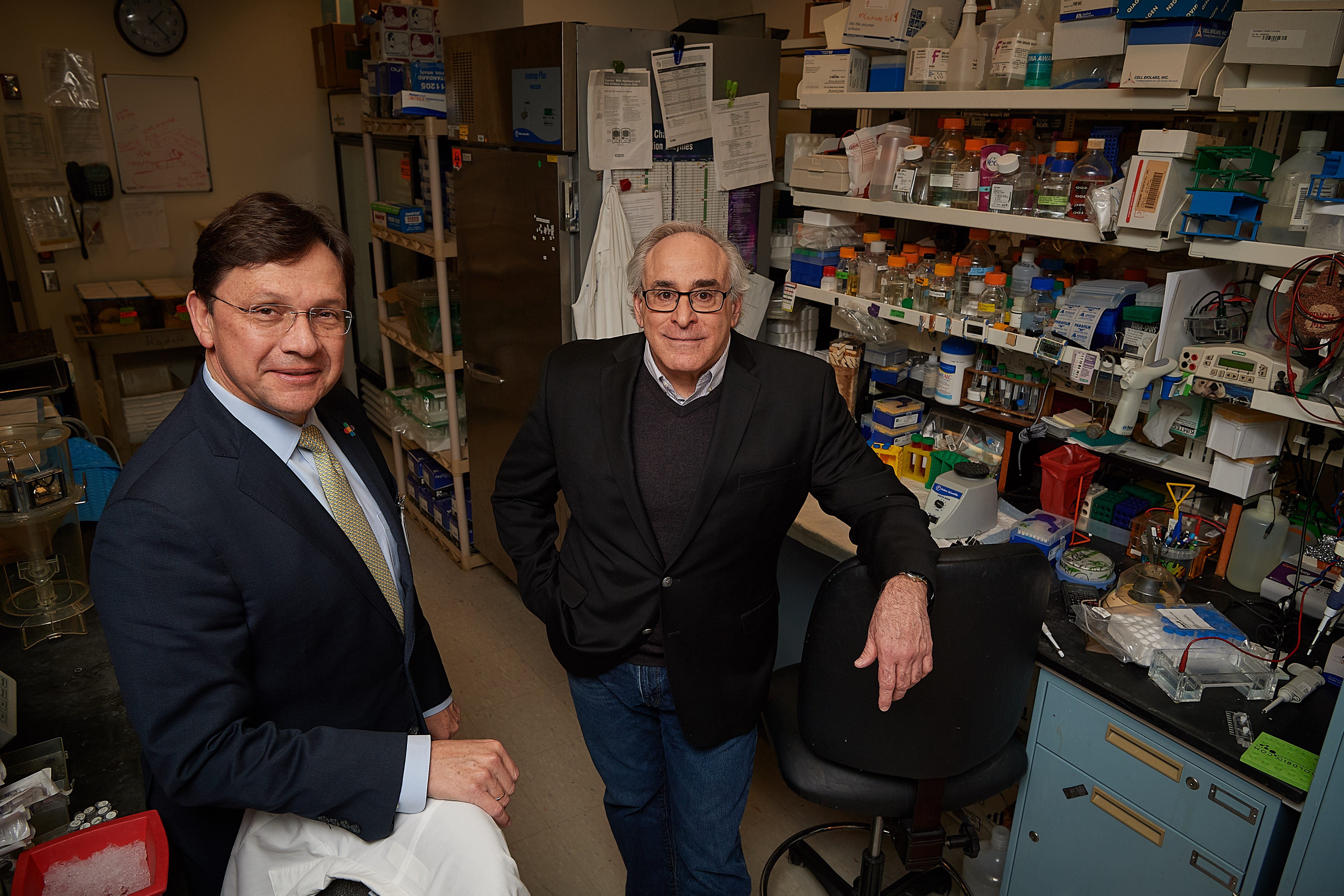
“An effective syphilis vaccine would represent a triumph for biomedical research over an ailment that has defied conventional public health strategies for prevention and control,” says Dr. Justin Radolf, professor of medicine and pediatrics at UConn School of Medicine and co-principal investigator with Dr. M. Anthony Moody of Duke University. “If successful, the scientific and public health impact of our approach will extend well beyond syphilis and establish a model to tackle other pathogens.”
Syphilis is primarily transmitted through direct contact with an infectious lesion during unprotected sex. Syphilis can also be passed from expecting mothers to their unborn children, with potentially devastating consequences for the health of the unborn child. Syphilis is the second leading cause of stillbirth and miscarriage worldwide. If left untreated, it can cause strokes, dementia, and other neurological diseases in any infected person.
Past attempts to control the syphilis epidemic by treating infected individuals and their partners have proved unsuccessful, since this approach is limited by many factors including difficulties diagnosing the disease, limited access to care for certain high-risk individuals, and resources for effective contact investigation. Furthermore, syphilis and HIV are recognized as “syndemics,” in which both infections can increase the risk of acquisition and transmission of the other.
The international study team is comprised of researchers from UConn School of Medicine, Connecticut Children’s Medical Center, the Duke Human Vaccine Institute, the University of North Carolina (UNC) at Chapel Hill Institute for Global Health and Infectious Diseases, UNC Project-Malawi, Masaryk University in the Czech Republic and Southern Medical University in Guangzhou, China.
“This center combines the unique capabilities of UConn Health’s Spirochete Research Lab with the rest of the study team, which has world-class vaccine research infrastructure, international health expertise, and unparalleled knowledge of bacterial genomics to achieve our long-term objective,” explains Juan Salazar, M.D., chair of pediatrics at UConn Health and physician-in-chief at Connecticut Children’s Medical Center.
The study team believes that the best vaccine candidates for syphilis will be found among the surface-exposed proteins within the outer membrane of Treponema pallidum (TPA), the bacterium that causes syphilis.
While TPA was identified over a century ago, only during the last 20 years have investigators made significant headway in identifying the proteins in the syphilis spirochete’s outer membrane. The UConn team, working within UConn Health’s Spirochete Research Laboratories, has been in the forefront of these efforts. The key breakthrough that laid much of the groundwork for the Cooperative Research Center (CRC) was the use of structural biology tools to identify proteins encoded within the spirochete’s genome predicted to form beta-barrels.
Three projects comprise the Cooperative Research Center. The first builds upon research conducted by Radolf with Melissa Caimano, associate professor of medicine and pediatrics at UConn Health. Project 1, which they describe as “immune-agnostic,” will select leading vaccine candidates based on bioinformatics, biophysical analysis, and structural modeling, regardless of whether they induce antibodies during the course of syphilitic infection in humans. Folded, recombinant forms of these proteins will be used to try to induce a protective immune response against TPA in immunized rabbits.
The second project, directed by Salazar and Arlene Seña, M.D., M.P.H., associate professor of medicine at UNC-Chapel Hill, and includes UConn Health researcher Kelly Hawley, Ph.D., takes its cue from the human immune system. Some individuals who contract syphilis go untreated due to missed diagnoses. Despite the lack of medical intervention, these individuals are usually able to control TPA infection over time. As a result, the research team believes that the surface-exposed portions of outer membrane proteins targeted by antibodies as part of the natural immune response to TPA infection could point to excellent vaccine candidates. This project will also establish a global clinical research consortium for syphilis vaccine development, by coordinating data and specimen collection from syphilis patients worldwide to catalog circulating spirochete strains.
The third project leverages technology developed for HIV research at the Duke Human Vaccine Institute. Armed with knowledge of the structures of TPA outer membrane proteins generated at UConn Health and Connecticut Children’s Medical Center, the Duke team, led by Moody, can identify B cells that produce antibodies directed against extracellular loops. The team then hopes to pull the antibodies out of isolated B cells and reengineer them using molecular techniques to increase their affinity for their targets, giving them an edge over the antibodies produced by the natural human immune response.
This grant is the culmination of years of work to set up a global-scale project, which required working closely with colleagues around the world. For the last 15 years, UConn Health researchers have partnered with health care providers at CIDEIM, an infectious disease research institute in Cali, Colombia. Thanks to the partnership, UConn Health scientists gained access to a large population of patients for their studies, and the doctors in Colombia received high-level training to recognize and treat syphilis. The on-going relationship has been a “win-win-win” for the researchers, clinicians, and patients.
For the new Cooperative Research Center, the partnership has expanded even further to Lilongwe, Malawi; Guangzhou, China and the Czech Republic with the help of researchers at the UNC Institute for Global Health and Infectious Diseases, Southern Medical University, and Masaryk University.
With patient specimens to be collected at five international sites on four continents, the researchers will be able to study geographically diverse strains of TPA in order to develop a comprehensive picture of the degree of variability of TPA’s outer membrane proteins. That knowledge will be critical to developing a vaccine or vaccines that can protect against strains circulating in different geographical locations.
Other Connecticut collaborators include Kelly Hawley, assistant professor, UConn Health & research scientist, Connecticut Children’s; Amit Luthra, instructor, UConn Health.
Other key project collaborators include Dr. Jonathan Parr, assistant professor, Division of Infectious Diseases, UNC, director of the Genomics Core; Dr. Jonathan Juliano, associate professor, Division of Infectious Diseases, UNC; David Smajs, professor, Masaryk University; Dr. Joseph Tucker, associate professor, Division of Infectious Diseases, UNC; Irving Hoffman, professor, Division of Infectious Diseases, UNC; Heping Zheng, vice director, Dermatology Hospital of Southern Medical University, Guangzhou; Dr. Bin Yang, chief, Dermatology Hospital of Southern Medical University, Guangzhou; Michael Weiner, vice president of molecular sciences, Abcam.
This research was supported by the NIH (Grant Number: NIH 1 U19 AI144177-01).